i waited for you in the park.
when you arrived,
you held me,
and your cold nose pressed against my neck.
you nuzzled me,
and our skin quickly
adapted to one another;
mine cooled, or yours warmed
i’m not sure.
i was happy and
excited about what we might become.
the sun and an early spring day
marked the passage of time
and life moving forward.
these were early days—before
waiting became an annoyance,
before illness,
when i didn’t understand what
holding my breath truly meant.
the anticipation of test results slowed time,
and hours in the treatment chair
felt like lifetimes.
after my first seizure,
when the illness forced my world apart,
time shifted.
you found me
coming to the emergency room
to gather the pieces.
fresh from outdoors,
from the chill of an early
chicago spring day,
remembering this:
your cold nose
pressing into my neck,
i can still feel it as time slowed.
and why can’t these moments
be eternity?
when two bodies
seek a common temperature,
can’t this search last forever?
Tag: cancer.org
The wind through an open door
At night, lying on my back, I stay awake and listen to the rattling of my lungs.
A wheeze, a strange resonating noise—like damp leaves—if mold had a sound, if abandoned rooms with winds spoke.
I insist I am okay.
I’ve always said, “I’m okay.”
From my youth, my father’s glare, to now, the groan of my lungs.
But I knew now I wasn’t; my body was revealing signs of sickness.
When had climbing a flight of stairs become a challenge?
Why was I losing weight?
Why did I wake up in the morning without the will to start the day?
The cravings of a young man—sexual longings, morning erections, and pleasuring myself in the stillness of the night—these were memories.
Someone my age shouldn’t be dealing with these issues, right?
I am a young man, strong and proud with rugged New England blood, generations of good health, and a life without doctors.
I kept telling myself, ‘Everything is okay.’
I kept repeating, “Everything will be okay.”
But it was never just an irritation in my throat.
The cough wasn’t just spring allergies.
“Hello,” I say.
“You are closer now.”
The wind through an open door has achieved form.
You have become a presence, a physical form I can’t ignore.
“Hello, Jeremiah.”
You’re in the hallway as a guest now, and you’ve even taken off your shoes.
How could I not welcome a guest?
A caller who had been inside, who had been within, was now at my door.
Cradling me as I sit on the shower floor, coughing blood into the drain.
Wrapping me in the steam of a scalding shower that never warms.
You are the fading winter, the arriving spring, and the buds on trees along West Thorndale.
You’re sitting next to me on the L.
Medical Alert ID
One of my biggest fears now, and since my diagnosis, is having a seizure. Obviously, I don’t want to have one anywhere/anytime, but my fear is that of having a seizure in public.
The vulnerability I feel when in the post-seizure state (“postictal”) is horrific. I don’t know where I am, who I am, who the people are around me, etc. Once, after a particularly intense seizure, both my mother and sister were sitting on my bed. Luckily, I was in bed at the time, so I didn’t hurt myself after losing consciousness. I frightened my sister so much and undoubtedly saddened her as well because, for the longest time, I just stared at her, unable to recall who she was.
A lot of the trauma I am currently working through with the help of my psychologist is the initial seizure. Currently, I can feel a seizure coming on. There are indications I’ve learned to recognize, often referred to as auras; these help me to take precautions so as not to fall and injure myself. In Chicago, when the first seizure occurred, I had no idea what was happening. I simply hit the deck. When I awoke, I could feel a rocking sensation and the hum and vibration of what I had come to understand as an engine. This knowledge didn’t help, as I had no sense of identity.
The paramedics had rummaged through my belongings and found my ID. This helped them understand who I was, but when they said “Mr. Ray,” I was unsure who or what they were referring to. “Mr. Ray, have you been doing drugs?” They asked this question repeatedly. I struggled, as I often do when regaining consciousness, and since they had no idea if I was, in fact, on drugs, they had me strapped down to the ambulance stretcher. Later, when in the ER, I discovered the cuts on my wrists from having struggled so much while in transport to the hospital. Again, they asked, “Mr. Ray, have you been doing drugs today?” I began to cry. “Mr. Ray, do you know what year it is?” I mumbled something, but I was unsure of what year it was. When I began to come around and gain a greater sense of who I was and where I was, I told them I was a graduate student studying in Chicago. I am sure the latter was evident in Chicago, but this helped them understand more. Finally, one of the paramedics said, “Ok, Mr. Ray, we’re going to untie your arms, ok?” Sometime later, well after I was in The ER, one of the paramedics came to see me. I didn’t recognize him, obviously. “Hi. Mr. Ray,” he said. I am sure he had found out, after inquiring about my toxicology report, that the only drug in my system was caffeine.
I currently wear a medical ID. This simply states that I suffer from grand mal seizures. This isn’t enough for me; I want it obvious that my medical condition is such that I was a cancer patient, and one of the ongoing ailments, perhaps an ailment for the remainder of my life, is seizures.
… I purchased the credit card-sized ID badge and a lanyard. As I gain more emotional and psychological confidence and the much-needed physical stamina, I hope to continue my walking routine, an oft-daily event that I greatly miss, which helps me process much of the events that have occurred over the past few years. I want the ID to be so evident that, should I have a seizure when out and about, my medical condition will be event, glaringly so. I have faith in my fellow man/womxn that, in such an event, I will be comforted and cared for until I regain a sense of who I am…
The thought of waking without knowing who I am, or even what I am, haunts me. The fear of being strapped down during this postictal time is even more so. The vulnerability, as mentioned, is so great that this prevents me from my outings — any outings, be they a trip to a cafe, to take in a movie, etc. I don’t want this fear to become so great that I avoid leaving the house. Currently, I can see this is where my fear and the ever-growing feeling of vulnerability are leading me.
The aluminum, bright red ID card, which I’ll wear around my neck on the outside of my clothing, will hopefully let me inch out more and more and break this paralyzing fear encroaching upon my life.

High-dose chemotherapy with (tandem) stem cell transplants


Where and how do I begin explaining high-dose chemotherapy with (tandem) stem cell transplants? I have been considering how I should go about describing the process. However, I wasn’t even sure I understood it correctly.
In my case, and this might be the same for other patients, I am not sure, but upon admittance, the clock starts at “day -5” (day negative 5). so “day 0” is when I return my stem cells. Days -5 — 0 are, as you might have guessed, chemo days. By this, I don’t mean normal outpatient days that, in my case, lasted several hours, depending on the regimen. No, I am talking about round-the-clock infusions, IV bags of chemotherapy drugs that run for 24 hours and then are switched out for new bags that run the same length for days and days. The intention, with such long days filled with heavy-duty chemo, is to destroy the current stem cells/marrow & annihilate the existing cancer and then replenish my system with untouched (by high dose chemo) stem cells from which my body will reconstruct itself literally from the ground up.
Along with the continuous stream of chemo, I have also been receiving liters upon liters of fluids. This is to prevent any damage to the liver, kidney & bladder. However, it is often uncomfortable, and, according to the nurse, I am currently retaining 8lbs/3.6kg of excess liquid. Needless to say, I feel uncomfortably bloated.
Between days -2 and 0, I will just be receiving mesna, a chemo protectant, and more fluids to continue to flush my filter organs.
2nd round
Tomorrow, August 4, 2017, I will return to Mass General Hospital for the second stem cell transplant. I am not ready; I want more time to rest and eat good (nonhospital) food to be “normal.” I don’t want to be inside for 2+ weeks, confined to a hospital floor, gazing longingly out of the windows, trying to imagine what the day feels like from a room that is kept at a constant temperature. In the back of my mind is the repetitive voice of reason explaining how this is needed and how “it’ll be over soon!” etc.
My beard is starting to grow again; it is darker and thicker in some areas and others, just thin indications of hair, translucent almost. Once more, I am surprised at how fast cellular regeneration occurs within the body and, as before, how willing it (the body) is to keep going and growing despite the near-constant bombardment of chemicals. I feel bad that, from tomorrow onward, my body will be fed these toxic chemicals and again will shed the newly grown hairs as the (chemo) agents destroy cells — both good and bad — all cells.
Again, the voice tells me it is for the best, this is about healing, “you’ll be well soon,”… etc.
When I was just a small child, I played in the woods near our house. For some reason, I consumed some berries growing wildly in the forest. As innocent as a child is, I just thought they were harmless and would taste yummy. When my mother heard it, she immediately called the doctor, who had the pharmacist deliver (yes, they delivered!) ipecac syrup. This is used to induce vomiting and administered if something potentially poisonous is ingested. Since my mother didn’t know what type of berries I had feasted upon, she assumed the worst. Naturally, she felt horrible when I vomited up what I could barely remember as a colorful, Pollock-like splatter of colorful berries (amongst other things recently consumed). I now feel the way my mother must have when she was trying to explain to me why I would feel poorly – and that it was for my safety – and that she was sorry – and that she loved me.
At night, or when first waking, I scan my body mentally from head to toe and envision myself embracing my own body as I explain why this must be endured – and that I’m sorry – and that I love it.
Check-in

I checked into Mass General today for what will be 1 of 2 stem cell transplants.
This will be a long summer & the realization of what I’m in for struck me when I started unpacking and settling in.
The Collection
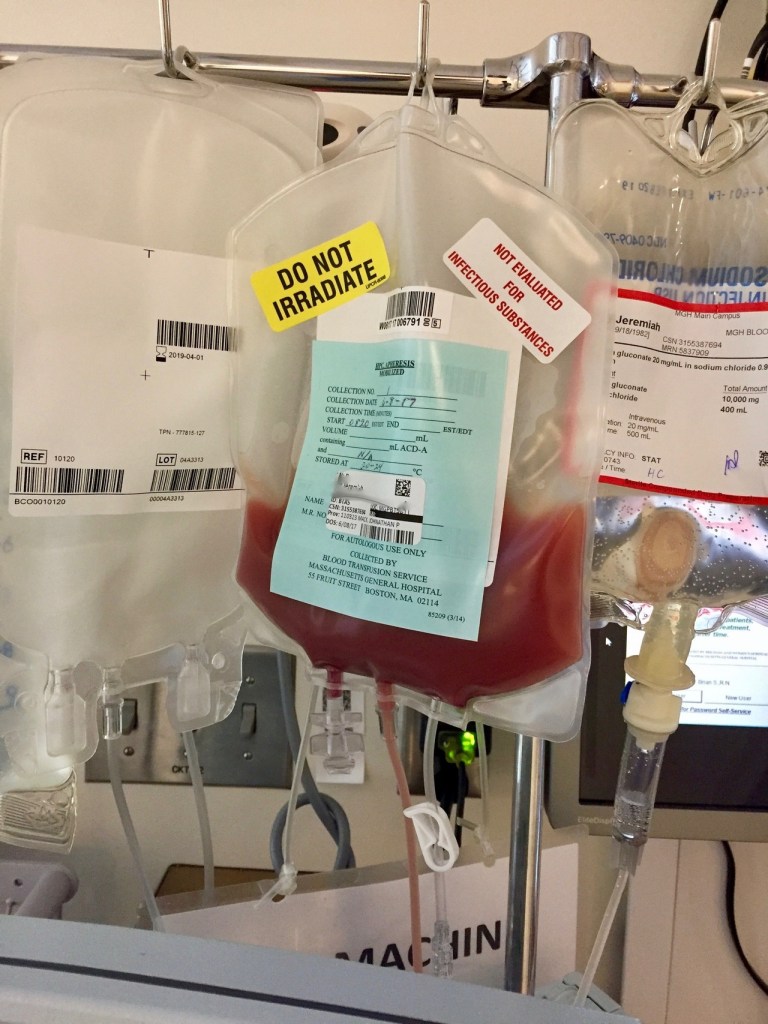

I spent the last five days in the hospital. During this time, I was receiving a continuous flow of IV antibiotics in an attempt to nip whatever was lurking in the bud to stay on track with an MGH/stem cell transplant. This didn’t go as planned when the fever spiked, and I missed the stem cell collection scheduled for Wednesday.
That afternoon (on Wednesday), while still hospitalized in Maine, the oncologist whose care I’m currently in at MGH called me. At this point, it seemed apparent that my fever was a result of neutropenia as well as from the filgrastim injections ( http://www.neupogenhcp.com/).
The blood drawn for cultures hadn’t, after 48 hours, indicated a blood-borne infection. The oncologist at MGH was convincing & practically demanded that I get discharged, drive down to Boston that afternoon/evening, and make the 07:00 Stem cell collection already on the books for the following day (Thursday, June 8). to me, this sounded reckless. I didn’t want to be in the hospital longer than needed, but I also was fearful of the big, germ-filled world waiting to sneeze on me and send me back to the ER. I feared that, should this happen, should my fever spike force me to the hospital for another 5 days or more, this would further delay the actual transplant. (something that has been postponed already due to cancer-related issues!) his fear was a different side of postponement & delay – that the small window of opportunity after the nadir (which refers to the lowest point that an individual’s blood cell count
will reach as a side effect of chemotherapy) & the peak reached as a result of the injections, would close on us. He was worried that if I didn’t make it Thursday to collect and thus left only Friday, we were taking a massive gamble as most people need at least two days to collect all the stem cells they will need for a transplant. If I were to wait until Friday and NOT gather all the cells, we’d have to finish on Monday and hope the injections were still assisting in generating the needed stem cells. It’s not only the shots that assist in this generation of cells! The whole reason for undergoing the monstrous round of chemo/etoposide was to send the body (after nadir) into white blood cell count overdrive! Add daily shots to the mix to assist this, and boom – massive (daily, maybe hourly?) jumps in cell counts.
So what did I do? I got discharged (June 7) and made the trip to Boston.
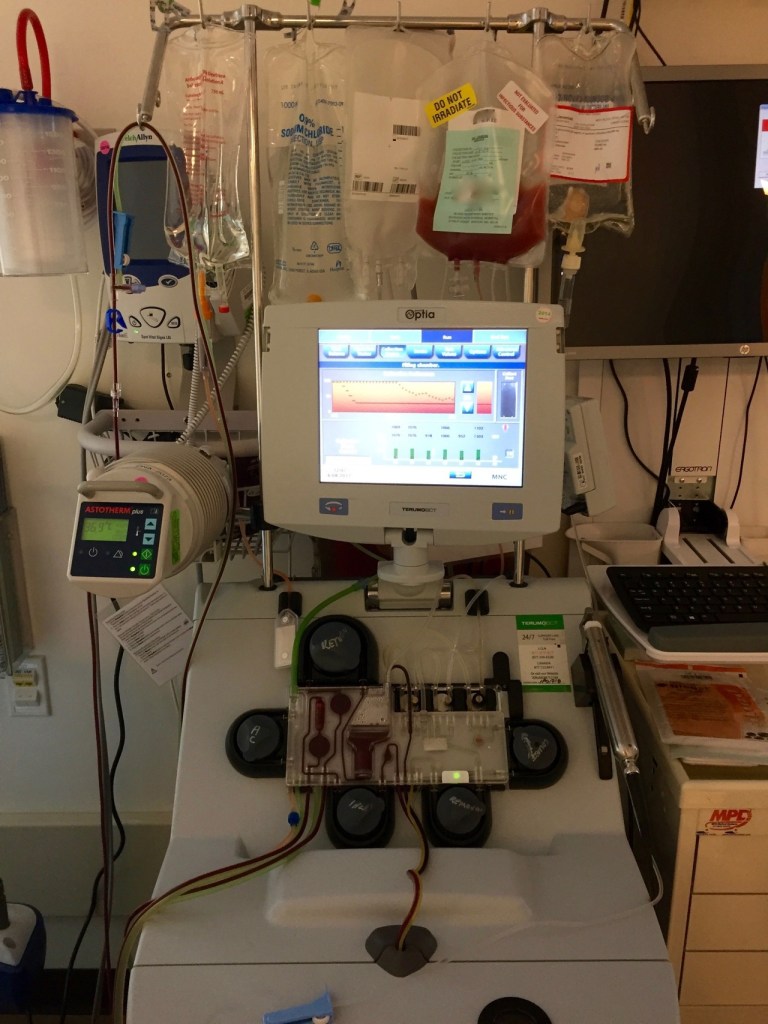
Today, June 8 (2017), at 07:00, I walked over to Mass General Hospital for collection. The process took several hours. My triple lumen pheresis catheter (seen in photos, the line coming out of my chest) worked perfectly!
When I was finally free, I took a much-needed stroll around the area to get fresh air and sunlight. I was awaiting a call from the nurse practitioner to tell me whether or not the collection was successful or if I needed to return the next day to finish up.
The plan worked, and, though one day off schedule, they gathered all the cells needed in one session.
Things change
This post contains images that some viewers might find disturbing.
Had things not changed, had everything stayed on course, I would have begun my first of two stem cell transplants today at Mass General Hospital (MGH). it is hard to believe it was over a week ago today I was rushed to the ER. Today, I clearly understand what is happening. At the time, however, I was in tears to the paramedics while en route trying to explain my health history in one long-winded sentence, as well as explain that currently, I couldn’t move my left arm.
… why am I still so surprised how fast things can & do change?
When I first met the neurosurgeon, he was optimistic that the 3.2cm lesion in my brain was merely causing swelling, pressing against a supplementary motor cortex (voluntary movement HQ). He was optimistic. However, his tone changed after steroids, administered to help decrease swelling when the lesion was discovered, didn’t assist in bringing back the slightest movement in my fingers or arm. I can hoist the weight of my arm using my shoulder, but there is no grip or dexterity in my fingers, hand, wrist, etc. & bending it at the elbow isn’t entirely possible on my own/without extra guidance from my right arm. It is the strangest thing to be looking at my fingers and telling them, asking them, and pleading with them to move, but they don’t. I still have sensations and can detect touch, warm/cool temps, etc. This is where the hope will reside for recovery of mobility & use.
Rather than just swelling from the lesion causing pressure, the surgeon feels part of the lesion (part of it) was pushing against one of the primary motor cortex bands that run along this particular section of the brain. I am still trying to wrap my head around this… but it explains the extremity’s continued immobility.
Future stem cell transplant steps are being postponed for a few weeks.
Naturally, there is a lot of healing to do in the meantime, and any immune-compromising regimen can’t be undertaken until later in the month. Even then, they may want to opt for radiation therapy, similar to what was used to address the first brain met, before moving forward with the stem cell transplant.
This physical limitation is proving more challenging to deal with than all the chemo hangovers thus far experienced.




The lesion
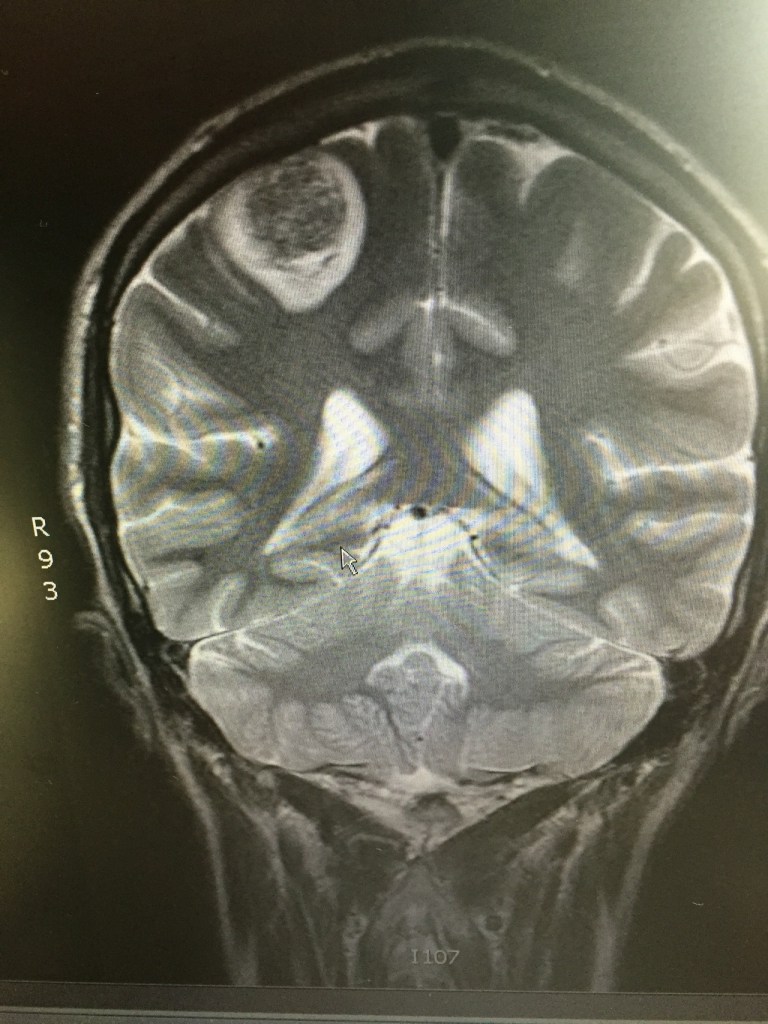

I should know this by now, but I don’t’; things change very quickly– alarmingly so.
The other day, I noticed that typing with my left hand was challenging. It wasn’t easy to access specific keys. Later that day, when attempting to play guitar, I again noticed that the fluidity with which I usually fingered the chords (using my left hand) wasn’t present.
The following day, while driving back from an appointment, I lost complete mobility in my left arm. Unsure if this was a seizure, a stroke…, or a clotting issue, my sister took me to the ER. As most of my ER stories go, they did several tests, the first of which, after vitals, was a head CT scan. What they discovered explained the loss of mobility/motor function in my left arm – a 3.2cm lesion on the back rear (right) lobe in and around the parietal and occipital lobe. (this is what I’m piecing together from the various doctors I’ve met. still trying to grasp the facts.) My MRI on Jan 30 showed no sign of this (what is assumed to be) metastatic spread. Unlike the other brain lesion that was dealt with using solely stereotactic radiosurgery (SRS) in early October (2016), this one will initially be surgically resectioned, and then SRS will be used. The main reason for that is its size.
This will most likely push back the stem cell transplant a few weeks or so, considering the healing time and then the radiation therapy afterward. That & this new and particularly aggressive/fast-growing brain met seem most urgent.
The surgical resection is scheduled for tomorrow, Apr 30, 2017.
Mystery to reality (a stem cell transplant)

To me, a stem cell transplant is still a mystery. I understand it theoretically, but it still seems like some sorcery. When I spoke briefly via phone with the doctor in charge of bone marrow/stem cell transplants at Mass General Hospital (MGH) before my appointment (April 20), it sounded like he wanted me to start the procedure the following day. There was this sense of urgency. I was, and am, ready. I needed the time (since being told of the recurrence) to accept and come to terms with it and thus prepare myself (on every level) for the next steps. Being “ready” on a purely medical level is accepting what is and the facts. Being “ready” on every other level only acknowledges the work and tasks ahead.
When initially diagnosed, I didn’t have time to think about everything, seek out other opinions, or talk to survivors and current patients in treatment. It was a seizure, hospitalization, surgery, and treatment. I understand that some of me was in denial when informed of the recurrence. Naturally. I also knew, from the crash courses I had given myself in oncology & cancer treatment (etc.), that, this time, I did have some time. As aggressive as my cancer may be, I knew I owed it to myself (and my body/mind!) to seek advice. Since all signs keep pointing back to this route, that of high-dose chemo with tandem stem cell transplants, I feel a sense of readiness. Also, and most importantly, I needed the time from my meeting with my oncologist (February 2) until I met with Dr. Einhorn (April 5) to not only research and explore but also cry, scream, and walk in circles in the woods (literally) to grasp it. In doing so, I unblocked and addressed some of which I didn’t have time to deal with initially when I was first diagnosed. Looking back, I am thankful for this time. Not only did I get to explore and look into the vast world of alternative therapies (clinical trials, studies, etc.). But I also had the pleasure of meeting (by phone, e-mail, or in person) some beautiful folks. On top of this, and perhaps most importantly, I got a better look at some of the emotions I “didn’t have time” to address before.
Anyways… those next steps, the preparatory stages, are even more complex than the (stem cell transplant) procedure itself, or so it seems. I suppose this makes sense, being that the very nature of a stem cell transplant (2 transplants in all) is so involved and brutal on the body that there needs to be adequate preparation. It’s not just relatively basic and seemingly simple stuff, like having my dentist sign off stating that any routine work has been done in their professional opinion is that my teeth are fine and ready, etc. It’s more timing and lining everything up so that it all is methodically prepped and in place that, like clockwork, it follows a pre-determined, pre-planned, pre-mediated schedule with such exactitude. I’ll break it down by posting updates as things move along.
Right now, the plan is to receive a single infusion of Etoposide on May
5th. Etoposide is a chemotherapy drug. I received it in various regimens during my initial treatment. The idea behind a single, stand-alone dose is to push the body into generating white blood cells to initiate a sort of overdrive in production. This is the body’s natural response under normal conditions while undergoing conventional chemo. Even though etoposide has cancer treatment and maintenance “benefits,” we’re using it to jump-start white blood cell production. After a two-day pause, just after the etoposide has flushed from my system and right when my body is in white blood) cell production, I will start giving myself daily white blood cell booster injections. I had these before; however, this was after the week of cisplatin-based therapy when my white blood cell was deficient & dangerously so. After 10 days of forcing my marrow into overdrive production, I’ll go in for harvesting.
Before high-dose chemo, which destroys my marrow, harvesting is done so there are adequate platelets to replenish that which is killed off by the high dose of chemotherapy.
Currently, all of these procedures will be done at MGH. I won’t be inpatient until I start high-dose chemo, as this will require a sterile, germ-proof environment.