i waited for you in the park.
when you arrived,
you held me,
and your cold nose pressed against my neck.
you nuzzled me,
and our skin quickly
adapted to one another;
mine cooled, or yours warmed
i’m not sure.
i was happy and
excited about what we might become.
the sun and an early spring day
marked the passage of time
and life moving forward.
these were early days—before
waiting became an annoyance,
before illness,
when i didn’t understand what
holding my breath truly meant.
the anticipation of test results slowed time,
and hours in the treatment chair
felt like lifetimes.
after my first seizure,
when the illness forced my world apart,
time shifted.
you found me
coming to the emergency room
to gather the pieces.
fresh from outdoors,
from the chill of an early
chicago spring day,
remembering this:
your cold nose
pressing into my neck,
i can still feel it as time slowed.
and why can’t these moments
be eternity?
when two bodies
seek a common temperature,
can’t this search last forever?
Tag: Jeremiah Ray Cancer patient
The “What-ifs”

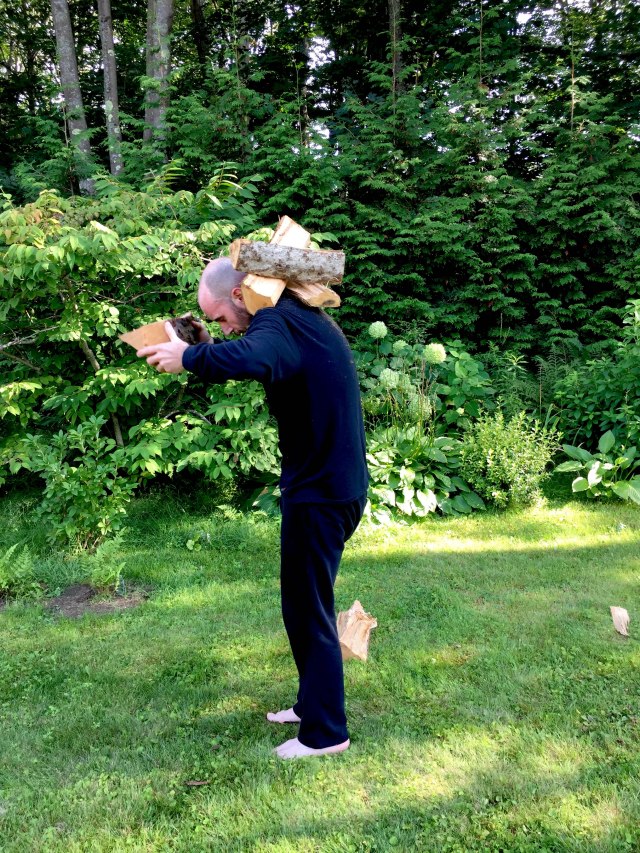
The weight carried,
the what-ifs upon bent backs –
(in) worry and (in) wondering,
“now? if not now, when?”
survivors hold this question;
they live in the moment
of continued burden.
how do I share the weight of gathered
memories?
how do I convey these worries?
I add them singly,
one by one,
layering them,
and bend my back to their weight,
asking,
“if not now, when?”




Discourse
I had a recent and brief exchange with my uncle after a recent post about life, its potential pointlessness, and the struggle to find meaning.

(Chris)
Interesting ruminations! I think that Tolstoy’s outlook is pretty pessimistic. I believe that life has a purpose, but I don’t necessarily
believe that your illness has anything to do with it. Your purpose may be to help someone later in life, maybe to have kids, work with people experiencing poverty, invent, write, or draw something important. Maybe this three-year period is just a detour that has nothing to do with that. I don’t know!!!
much love,
(Jeremiah)
His outlook certainly was pessimistic… but I feel that was the impetus for his spiritual pursuits/awakening. He had to fall into that place of despair to arrive. I guess, the way I look at it, I was already en route to these things; in my last semester of grad school, I was going through interviews with the Peace Corps to work (with people with low incomes, perhaps) in Albania. I was writing … I was drawing. I think that a detour that goes on for three years is a bit excessive. It isn’t the physical journey but that of the mind, psyche, etc. As I have written, the toll that all this has taken is very significant. Yes, my oncologist can say, “You look great!”
But he doesn’t see the damage on the inside. Of course, his objective is to treat the patient, so externally, I look “great.” I don’t know where I am going with this. I do that this illness, and the longevity of it, MUST have something to do with it / with life. I have to think like this; otherwise, what’s the point? If all my struggling physically and psychologically was all for naught … I can’t go that route in thinking… I spiral out of control…
Chris
Naturally, everything we go through leads us to be who we are at any moment. So you are, and will be, a very different person than you would have been had you not gotten cancer. But that doesn’t mean (in my mind) that it is directly related to your purpose in life.
Medical Alert ID
One of my biggest fears now, and since my diagnosis, is having a seizure. Obviously, I don’t want to have one anywhere/anytime, but my fear is that of having a seizure in public.
The vulnerability I feel when in the post-seizure state (“postictal”) is horrific. I don’t know where I am, who I am, who the people are around me, etc. Once, after a particularly intense seizure, both my mother and sister were sitting on my bed. Luckily, I was in bed at the time, so I didn’t hurt myself after losing consciousness. I frightened my sister so much and undoubtedly saddened her as well because, for the longest time, I just stared at her, unable to recall who she was.
A lot of the trauma I am currently working through with the help of my psychologist is the initial seizure. Currently, I can feel a seizure coming on. There are indications I’ve learned to recognize, often referred to as auras; these help me to take precautions so as not to fall and injure myself. In Chicago, when the first seizure occurred, I had no idea what was happening. I simply hit the deck. When I awoke, I could feel a rocking sensation and the hum and vibration of what I had come to understand as an engine. This knowledge didn’t help, as I had no sense of identity.
The paramedics had rummaged through my belongings and found my ID. This helped them understand who I was, but when they said “Mr. Ray,” I was unsure who or what they were referring to. “Mr. Ray, have you been doing drugs?” They asked this question repeatedly. I struggled, as I often do when regaining consciousness, and since they had no idea if I was, in fact, on drugs, they had me strapped down to the ambulance stretcher. Later, when in the ER, I discovered the cuts on my wrists from having struggled so much while in transport to the hospital. Again, they asked, “Mr. Ray, have you been doing drugs today?” I began to cry. “Mr. Ray, do you know what year it is?” I mumbled something, but I was unsure of what year it was. When I began to come around and gain a greater sense of who I was and where I was, I told them I was a graduate student studying in Chicago. I am sure the latter was evident in Chicago, but this helped them understand more. Finally, one of the paramedics said, “Ok, Mr. Ray, we’re going to untie your arms, ok?” Sometime later, well after I was in The ER, one of the paramedics came to see me. I didn’t recognize him, obviously. “Hi. Mr. Ray,” he said. I am sure he had found out, after inquiring about my toxicology report, that the only drug in my system was caffeine.
I currently wear a medical ID. This simply states that I suffer from grand mal seizures. This isn’t enough for me; I want it obvious that my medical condition is such that I was a cancer patient, and one of the ongoing ailments, perhaps an ailment for the remainder of my life, is seizures.
… I purchased the credit card-sized ID badge and a lanyard. As I gain more emotional and psychological confidence and the much-needed physical stamina, I hope to continue my walking routine, an oft-daily event that I greatly miss, which helps me process much of the events that have occurred over the past few years. I want the ID to be so evident that, should I have a seizure when out and about, my medical condition will be event, glaringly so. I have faith in my fellow man/womxn that, in such an event, I will be comforted and cared for until I regain a sense of who I am…
The thought of waking without knowing who I am, or even what I am, haunts me. The fear of being strapped down during this postictal time is even more so. The vulnerability, as mentioned, is so great that this prevents me from my outings — any outings, be they a trip to a cafe, to take in a movie, etc. I don’t want this fear to become so great that I avoid leaving the house. Currently, I can see this is where my fear and the ever-growing feeling of vulnerability are leading me.
The aluminum, bright red ID card, which I’ll wear around my neck on the outside of my clothing, will hopefully let me inch out more and more and break this paralyzing fear encroaching upon my life.

“Living one day at a time…”

I have had quite a few appointments in the last couple of weeks. I met with my oncologist, and we spoke about the recent MRI. The swelling of the initial lesion in my brain is still stable! As with before, stability is good — excellent! We’ve scheduled another MRI for two months out (mid/late February). With this continued stability, it is unlikely to swell, or continue to swell, more. Though, I am not entirely sure.
I also had a meeting with my neurologist. This was more revealing than the MRI results. As you recall, I wore the ambulatory EEG for 72 hours. All the diodes on my head were connected to a small box I wore around my waist. If any “strange” sensations or feelings arose, I was to press a tiny button on the side of the box. On the EEG reading, this will simply make a note of a specific time, and then, when the neurologist goes over the entire reading, they can go directly to these points and “see” what sort of brain activity was occurring at these specific times.
I pressed the button a total of 33 times over 72 hours. If, for example, I felt slightly dizzy or even disoriented, I pressed the button. I often have these moments when the world seems very distant, or I seem removed from the world. This is very, very difficult to explain. I have tried to articulate it several times. I have taken a step back and am watching the world — an “out of body” experience. This sensation has been so unnerving in the past that I have gone to the emergency room several times.
I was curious how these moments (the “out of body” sensations) would appear on the EEG reading. I was sure that these were some sort of petit mal seizure activity. According to the epilepsy foundation, petit mal seizures, an older term for “absence seizure”, are a type of seizure that causes a sort of lapse in awareness. “Absence seizures usually affect only a person’s awareness of what is happening at that time, with immediate recovery… The person suddenly stops all activity. It may look like he or she is staring off into space or just has a blank look.” This, more or less, sums up the feelings and sensations wherein I am removed from the world, that “out of body” sensation. When I wore the ambulatory EEG (72 hours), I experienced several of these occurrences.
However, nothing on the EEG reading indicated any abnormal brain activity. For 72 hours, everything appeared as it should. Granted, over these 72 hours, there was no reduction of anticonvulsant medication or any other means that, during an inpatient stay for monitoring, a seizure would be provoked. Nonetheless, during these times of “unnerving” sensations (again, the “out of body” experience), nothing out of the ordinary appeared.
This came as a total shock to me. I explained these strange feelings to my neurologist, as I have done in the past, but he again confirmed the results of the ambulatory EEG reading — a reading reviewed by several doctors.
This being the case, he wants to hold off on the inpatient stay for monitoring. “Let’s leave ‘well enough alone,’ Jeremiah.” Again, I pressed him, trying to find answers. I wanted him to pinpoint the reason behind these sensations and explain what was going on within me in plain and simple terms. “… anxiety, most likely, stress, PTSD… a sort of ‘depersonalization'”. This is also the theory of depersonalization that my psychologist holds.
These terms seem so vague. I was expecting to go to my appointment and hear that reading was indicative of these factors; an inpatient stay for monitoring was next in line, and then, after confirmation of particular, definitive activity, brain surgery would follow. My oncologist assured me I didn’t want brain surgery, as does my neurologist. In fact, my neurologist stated rather bluntly that I was to “leave the brain alone!” I insisted that brain surgery wasn’t frightening or an issue as I’ve already had it once. Due to my lack of any formal medical training, my pleas went unheard.
I understand why. Of course, who wants to tamper with the brain — especially this left frontal lobe area where the former lesion is located? When a neurologist and neurosurgeon insist that surgery isn’t an option or an option they are very reluctant to consider, who am I to offer an argument?
It isn’t so much that I want to be seizure-free, though that would be ideal; it is that I want answers. I want to know why; why this and why that. The seizures are just one thing I can fixate on when the larger question is, “Why did any of this happen in the first place?” I want to know why! Why can’t one of these doctors give me a solid answer with all their (western) medical knowledge and years of experience?
I am learning acceptance. I have come a long way in letting go and embracing the unknown over these years. On certain days, today, for example, I can sit with tea in hand and watch the sun slowly migrate across the wall, and there is this peace here.
American theologian Reinhold Niebuhr wrote a sermon concerning this. Though it is best known for its initial/opening lines, it is the second part that, upon rereading it, really strikes a chord with me.
“Living one day at a time,
Enjoying one moment at a time,
Accepting hardship as a pathway to peace…”
I am desperately seeking reasons for this hardship. In doing so, I fear this endless pursuit will overshadow life’s most straightforward, profound, and poetic aspects.
Today, as mentioned, with tea in hand and watching the sun gain its strength each day, I am okay with it — with everything.
PTSD
A few days ago, I decided to check my temperature. I was sniffling, probably due to seasonal allergies, but I was also concerned I might have a cold after taking my temperature, which rested nicely at around 98.6F. I took out an alcohol swab to wipe the end of the thermometer.
Immediately after removing the single-use swab from the packet, the pungent aroma wafted. Shaking almost uncontrollably, I made my way unsteadily to the foot of my bed. There, I continued to tremble, a jittery sensation as though I had consumed too much caffeine. My body warmed, almost a flushing feeling. My knee-jerk reaction in such a situation is to reach for an Ativan.
I was worried I might be too unsteady on my feet, so I chose to remain seated. My reaction, which I now understand to be a “trigger,” was activated by the smell of the alcohol swab. I felt nauseated while sitting on the edge of the bed, but I tried to calm myself by focusing on my breathing and posture. I’ve been practicing this mindfulness technique with the help of my therapist in such situations. Although I have Ativan as a backup, I don’t want to rely on it constantly. I managed to breathe through the intense anxiety, and slowly, it began to dissipate. However, it was followed by extreme fatigue, as usual.
While at Mass General, I had my temp taken regularly, every time vitals were taken. After this, the nurse on duty would wipe the thermometer. It was sterile, just like everything else in my isolated room. So great was the need for precaution that for both my transplants, I saw only the eyes of the nurses, doctors, and visitors as surgical masks shielded their faces. It is tangential, but it does illustrate the necessity for sterility and the regular use of alcohol swabs and other such disposable cleaners.
I have had numerous experiences such as this: legs shaking while at a clinic, nausea during routine blood work, and extreme panic while in an MRI machine. The list goes on and on and on…
I have strayed away from the term “Post Traumatic Stress Disorder,” though I am not sure why. In many ways, I thought it was reserved for people who had experienced events that were far more traumatizing. I also didn’t want to label it, especially that one. I didn’t want to see myself as traumatized. I didn’t want to be in that place. When I was first diagnosed, I hoped to go to the clinic for a few months of treatment and then return to my everyday life. Admitting that I was traumatized would mean needing more treatment, not physical therapy, but rather addressing the ongoing effects of cancer once the initial battle was over.
My psychologist and I have spent numerous hours both addressing aspects of trauma, how it looks and feels, etc., and also skirting the subject altogether. We’ve danced around it, so to speak, but also avoided entirely that which has been glaring at me, lurking, waiting for me to address it and growing larger each day I didn’t.
I thought of trauma as something that held someone back, something that was fixed in a specific time/place. I thought it was an event that never released its talons, rendering someone helpless & forever there, reliving the past events. I didn’t want that. I am embarrassed to admit I thought I was too strong. The idea above, that of strolling into the clinic and strolling back out after a few months, was how I saw myself. After the completion of my second stem cell transplant, and I was a few days away from being discharged, my oncologist said, “Well, you’ve really trooped through these!” That was me, the warrior. I only let my guard down in front of a few select nurses. I held my tears back until I was in the bathroom, supposedly showering; I’d turn on the water and then sit there crying. At night, I would slip into weird, psychedelic dreams, from which I would wake up moaning, curled into a fetal position, clutching my stuffed animal with such force my fingers would ache the next day.
This is fear. This is pain. This is trauma.
I see the label of PTSD as synonymous with being stuck somewhere in the past, reliving it over and over. The truth is, I have barely, if at all, even begun to let myself do that. To relive and work through an event(s) of significant trauma, pain, sadness & anger is, in fact, stronger. When an alcohol swab sends someone into a tailspin, into a place of panic because of the memory it holds, it is evident that something needs to be addressed, something needs to be unpacked.
I have been told that life post-cancer treatment is the most difficult; it is when the real work begins. It is when things rise to the surface and demand to be addressed. If not, they will have their talons firmly fixed into their prey, and one will be held there forever, somewhere in the past.

I’m not going to die…
I’m not going to die, at least not yet.
When my oncologist said, “There is some swelling around the former tumor in your head. This might be the tumor waking up, but we’re not sure right now.”He then mumbled something else, which now escapes my memory, as things do when you’re told such news. Then I mumbled something in response, neither of us wanting to address reality, just mumbling a language that we both agreed upon but neither spoke fluently.
I had several days to mull this over in my mind. It was the longest several days of my life. I played out every possible scenario, walked them all to the end of my imagination, and then started with a new possibility and led that one down the same road. A tumor that had potentially “woken up” and presented with edema (swelling) around it.
Sure, here is the revised text:
I found myself constantly thinking about death. Despite being told that my body could handle more chemotherapy, I questioned whether I really wanted it. After undergoing extensive chemotherapy, did I want to endure more? In addition, I was still dealing with numerous chemotherapy-related issues such as neuropathy, tinnitus, dizzy spells, extreme fatigue, memory problems, slight speech impairment, nightmares, anxiety, and depression. Could I really handle more? Moreover, would additional chemotherapy be effective? Would it only prolong my life without actually curing this disease?
The day before my MRI, I sat on our porch, basking in the beauty of the world around me. The gentle buzz of bees filled the air as they industriously collected pollen from the vibrant flowers. Watching their instinctual knowledge of which blooms were nearing their end was fascinating. I was struck with the realization that we are on a ceaseless quest to evade the inescapable fate of mortality – even more so, the recognition of it.
I truly and honestly looked at death in that glorious sunshine on the porch amidst the bees and butterflies. It wasn’t some philosophical idea, some existentialist pondering, but a cold-hearted fact of what I thought was fast approaching. For the first time since the beginning of all this, since my seizure in Chicago to the most recent comment made by my oncologist about a tumor possibly waking up, I felt okay about it. I felt Okay about the possibility of dying. More importantly, I felt at peace with it.
Even now, writing the words is hard to fully express. Words fall so incredibly short. It is not that I was resigned or apathetic. It wasn’t that death was a welcomed reprieve from the madness of my life that, when it finally arrived, I would ask, “What the fuck took you so long?” It’s that death, the possibility of dying, the likelihood that it would arrive soon, graced me with a profound inner peace, one that I have never before felt in my life.
I didn’t want to move. I didn’t dare shift my gaze out of fear that this would disrupt the sensation and overall feeling I was currently blessed with.
“Hi Jeremiah, this is Dr. _; it looks like the swelling is due to necrosis, a cellular death that can occur after radiation. We’ll just keep track of it; I’ll schedule you for an 8-week follow-up. I don’t think surgical resection is needed, but I’ll put you in touch with a neurosurgeon, and they can go over that with you.
… and that’s it, necrotic tissue causing swelling.
There is a lot of work to be done now. One year post stem cell transplant allows for little breathing room, but that’s plenty for me — that’s more than enough. The real struggle now is with my mind and heart; the PTSD, anxiety, etc., will just take time and patience and love — self-love especially. The level of peace, however, and the acceptance I felt on that day, and still feel now, will go a long, long way in my emotional & psychological recovery. In using the metaphor of one of my latest posts regarding my feeling of helplessness & exhaustion being like the crashing waves under which I’m struggling to stay afloat, I can touch the sea floor now. Also, the land is clearly visible, and the tide finally works in my favor.
Birthdays

Birthdays are always an interesting point of reference to look back at time. They make a good starting place to look at a swath of years and note changes, growth, etc., to take one birthday, jump backward to the previous year, and look at the space in between.
On September 18, 2017, I turned 35 years old. Initially, I was not excited about the approaching birthday as the years from 33 ½ to 35 (from diagnosis to present) were lost for lack of a better term. This was my mentality leading up to the day — that that time was irreplaceable, gone, etc.
There are two ways to view this: as time being lost, with those years and months of being sick and in and out of treatment, or as something relative. I wasn’t even sure I would live to see my recent birthday. During the last round of high-dose chemo, when I was at the lowest point imaginable, I asked the night nurse if I was going to die. Feeling as I did, I was sure I wouldn’t live to see the following day, let alone my 35th birthday, which was only a matter of weeks away. Thus, the relativity of age, years, and time.
I awoke on my 35th birthday feeling more positive and ready — I had lived to see the day.
I’ve been trying to avoid dwelling on the past and revisiting the years before my diagnosis. However, I can’t help but remember significant moments, like birthdays, that were not overshadowed by poor health. Time now feels like it’s split into two distinct sections: before and after my diagnosis. But in reality, time doesn’t work that way; life is a mix of moments and events that all come together. Focusing on the present and fully embracing our current moments is essential. While there are events I wish I could erase from my memory, it’s impossible to pick and choose our experiences selectively. Who would we be without these moments, both good and bad? Who would we be without the nights we thought we wouldn’t survive and the mornings that surprised us by arriving?
The Collection
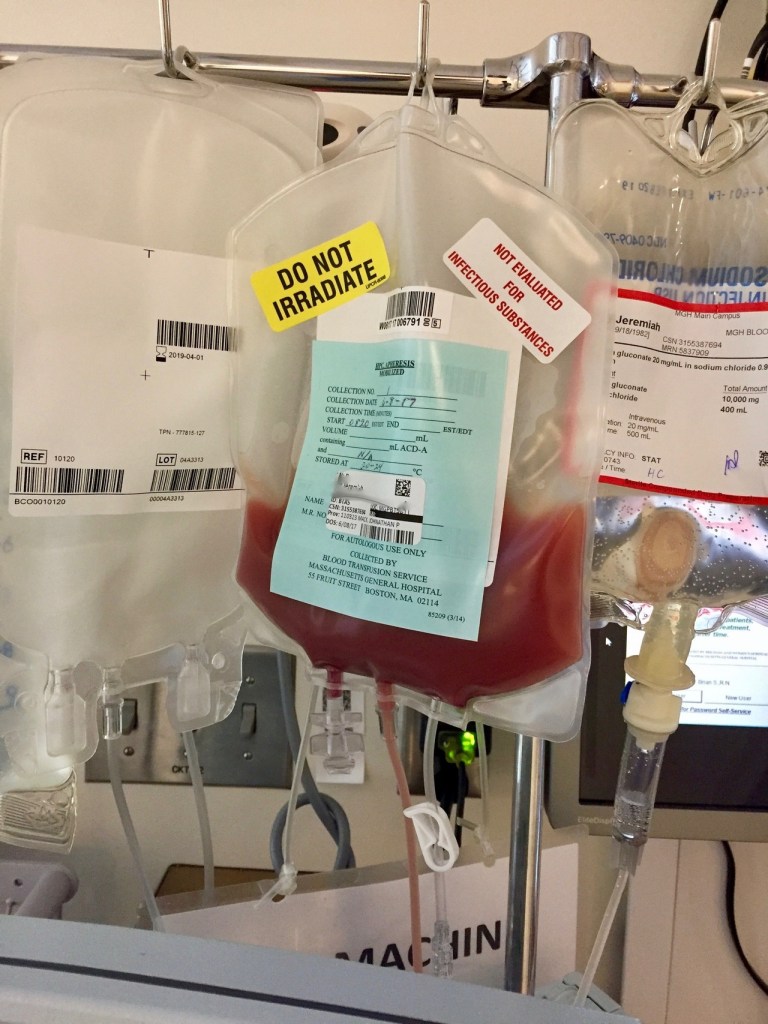

I spent the last five days in the hospital. During this time, I was receiving a continuous flow of IV antibiotics in an attempt to nip whatever was lurking in the bud to stay on track with an MGH/stem cell transplant. This didn’t go as planned when the fever spiked, and I missed the stem cell collection scheduled for Wednesday.
That afternoon (on Wednesday), while still hospitalized in Maine, the oncologist whose care I’m currently in at MGH called me. At this point, it seemed apparent that my fever was a result of neutropenia as well as from the filgrastim injections ( http://www.neupogenhcp.com/).
The blood drawn for cultures hadn’t, after 48 hours, indicated a blood-borne infection. The oncologist at MGH was convincing & practically demanded that I get discharged, drive down to Boston that afternoon/evening, and make the 07:00 Stem cell collection already on the books for the following day (Thursday, June 8). to me, this sounded reckless. I didn’t want to be in the hospital longer than needed, but I also was fearful of the big, germ-filled world waiting to sneeze on me and send me back to the ER. I feared that, should this happen, should my fever spike force me to the hospital for another 5 days or more, this would further delay the actual transplant. (something that has been postponed already due to cancer-related issues!) his fear was a different side of postponement & delay – that the small window of opportunity after the nadir (which refers to the lowest point that an individual’s blood cell count
will reach as a side effect of chemotherapy) & the peak reached as a result of the injections, would close on us. He was worried that if I didn’t make it Thursday to collect and thus left only Friday, we were taking a massive gamble as most people need at least two days to collect all the stem cells they will need for a transplant. If I were to wait until Friday and NOT gather all the cells, we’d have to finish on Monday and hope the injections were still assisting in generating the needed stem cells. It’s not only the shots that assist in this generation of cells! The whole reason for undergoing the monstrous round of chemo/etoposide was to send the body (after nadir) into white blood cell count overdrive! Add daily shots to the mix to assist this, and boom – massive (daily, maybe hourly?) jumps in cell counts.
So what did I do? I got discharged (June 7) and made the trip to Boston.
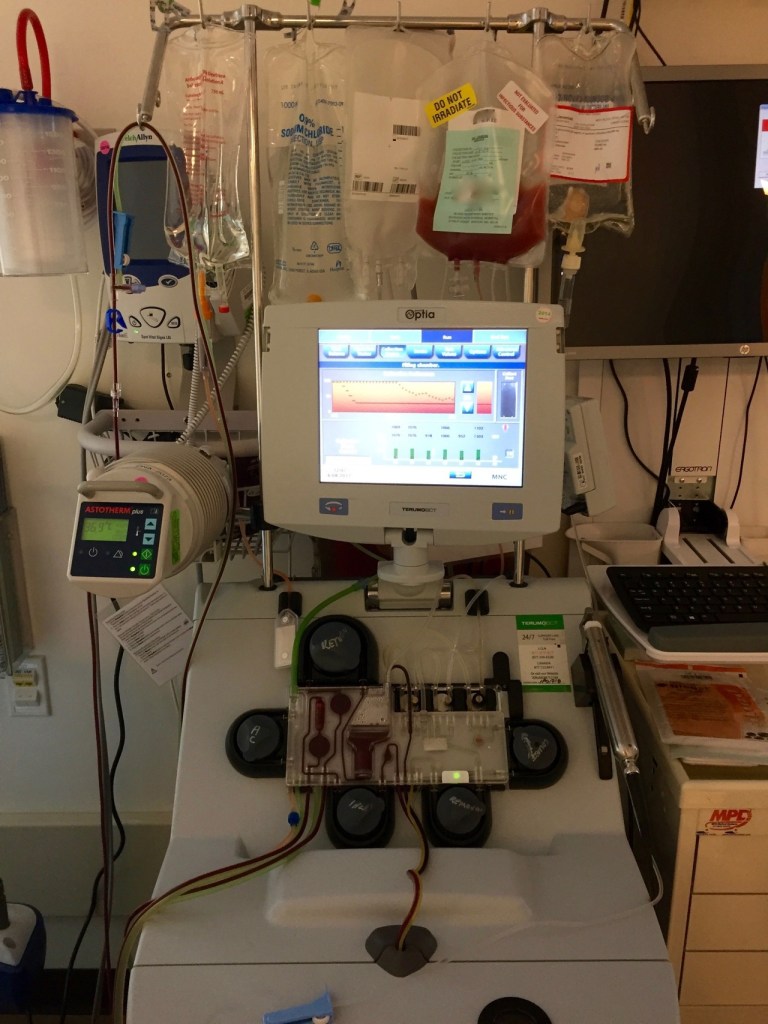
Today, June 8 (2017), at 07:00, I walked over to Mass General Hospital for collection. The process took several hours. My triple lumen pheresis catheter (seen in photos, the line coming out of my chest) worked perfectly!
When I was finally free, I took a much-needed stroll around the area to get fresh air and sunlight. I was awaiting a call from the nurse practitioner to tell me whether or not the collection was successful or if I needed to return the next day to finish up.
The plan worked, and, though one day off schedule, they gathered all the cells needed in one session.
Things change
This post contains images that some viewers might find disturbing.
Had things not changed, had everything stayed on course, I would have begun my first of two stem cell transplants today at Mass General Hospital (MGH). it is hard to believe it was over a week ago today I was rushed to the ER. Today, I clearly understand what is happening. At the time, however, I was in tears to the paramedics while en route trying to explain my health history in one long-winded sentence, as well as explain that currently, I couldn’t move my left arm.
… why am I still so surprised how fast things can & do change?
When I first met the neurosurgeon, he was optimistic that the 3.2cm lesion in my brain was merely causing swelling, pressing against a supplementary motor cortex (voluntary movement HQ). He was optimistic. However, his tone changed after steroids, administered to help decrease swelling when the lesion was discovered, didn’t assist in bringing back the slightest movement in my fingers or arm. I can hoist the weight of my arm using my shoulder, but there is no grip or dexterity in my fingers, hand, wrist, etc. & bending it at the elbow isn’t entirely possible on my own/without extra guidance from my right arm. It is the strangest thing to be looking at my fingers and telling them, asking them, and pleading with them to move, but they don’t. I still have sensations and can detect touch, warm/cool temps, etc. This is where the hope will reside for recovery of mobility & use.
Rather than just swelling from the lesion causing pressure, the surgeon feels part of the lesion (part of it) was pushing against one of the primary motor cortex bands that run along this particular section of the brain. I am still trying to wrap my head around this… but it explains the extremity’s continued immobility.
Future stem cell transplant steps are being postponed for a few weeks.
Naturally, there is a lot of healing to do in the meantime, and any immune-compromising regimen can’t be undertaken until later in the month. Even then, they may want to opt for radiation therapy, similar to what was used to address the first brain met, before moving forward with the stem cell transplant.
This physical limitation is proving more challenging to deal with than all the chemo hangovers thus far experienced.



