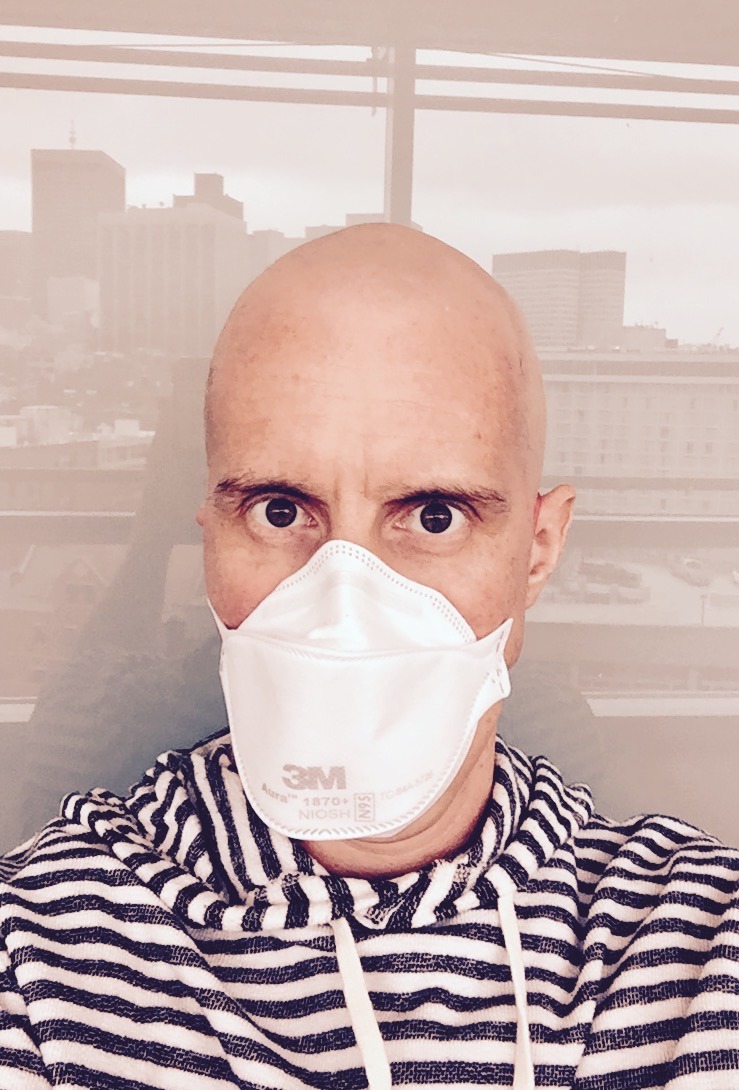
“Stress, trauma, and unexpected life developments — such as a cancer
diagnosis, a car accident, or a layoff — can throw people off stride
emotionally and mentally. Writing about thoughts and feelings that arise
from a traumatic or stressful life experience — called expressive
writing — may help some people cope with the emotional fallout of such
events. But it’s not a cure-all, and it won’t work for everyone.
Expressive writing appears to be more effective for people who are not
also struggling with ongoing or severe mental health challenges, such as
major depression or post-traumatic stress disorder.”
It sounds like I am beating a dead horse when I talk about “getting over” things. In many ways, and I do recognize this, I am. It isn’t that I’m obsessed with this idea, or beating myself up… it is simply that I am trying to come to terms, accept, move onward.
My fear is, and this too might be glaringly obvious, I worry about getting stuck there. Perhaps this is why I’m so keen on stepping forward and into the present.
I ruminate. I think and overthink and re-think… I try to work something out, see it from every angle and point of view. This has served me well and has helped in many ways. However, in regards to cancer and cancer treatment, I worry that it might be too great a focal point.
The above quote, published by Harvard Health, interests me. I fancy myself a wordsmith, even though my spelling and grammar are rather questionable (thank you neurotoxicity!). With writing, especially that which isn’t fiction, I grapple with subjects and, as with my other rumination skills, pick at it, dissect it, scrutinize it.
What I’m beginning to understand, and this quote really gets to the heart of it, is that my trauma from these many experiences had over the past two years, might be hindering me from working through something and thus letting it go. (Perhaps I am even overthinking this…)